Decision of the Laureates of the Fifth Hideyo Noguchi Africa Prize
The Government of Japan has decided to award the Fifth Hideyo Noguchi Africa Prize to Dr. Abdoulaye Djimdé (Republic of Mali) for Medical Research Category, and Drugs for Neglected Diseases initiative (DNDi) for Medical Services Category.

Medical Research Category
Dr. Abdoulaye Djimdé (Republic of Mali)
Born in the Republic of Mali in 1964. 61 years old. Researcher specialized in molecular parasitology. Obtained Pharmacy Doctorate at the National School of Medicine and Pharmacy Bamako, Mali and Philosophy Doctorate at the University of Maryland, USA.
Current Director, Malaria Research and Training Center, University of Science, Techniques and Technologies of Bamako. (Photo credit: Abdoulaye Djimdé)
Reasons for Award
The tragic experience of losing a sibling to malaria as a child and his initial career as a young pharmacist motivated Dr. Djimdé to pursue research on malaria, an endemic disease threatening the lives of people in Africa. The results of his research over the past thirty years have contributed significantly to improved treatment and control of malaria and have had an important impact on the health policies of African governments and the WHO. In particular, Dr. Djimdé, together with collaborators, had shown that the Plasmodium falciparum gene that conferred chloroquine resistance in laboratory strains was responsible for chloroquine-resistant malaria in malaria patients through his field research in malaria-endemic areas of Mali. He went on to design molecular markers that can confirm chloroquine resistance in the field. He also demonstrated the safety and efficacy of antimalarial drugs through clinical trials of artemisinin-based combination therapies. Furthermore, he established the Pathogens genomic Diversity Network Africa (PDNA), a collaborative research network for malaria control among 12 African countries (currently 16 countries) and built a system for sharing experimental protocols and genetic data. In addition, as director of the Malaria Research and Training Center (MRTC) at the University of Science, Techniques and Technologies of Bamako, he has worked diligently to train young scientists and has collaborated with many international research groups. By doing so– despite diverse challenging conditions– he has developed the center into a central hub of an international network of malaria research. Through these accomplishments, his research has saved the lives of many people living in malaria-endemic areas, and he remains firmly committed to realizing the dream of a “malaria-free Africa.”
Summary of Achievements
Despite recent progress, malaria remains one of the most pressing public health problems in sub-Saharan Africa. Growing up in rural Mali, Dr. Abdoulaye Djimdé had a firsthand tragic experience with this terrible disease, which took the life of one of his beloved brothers, when he was just 12 years of age. This experience moved him to become an anti-malarial scientist later in life and prevent other children from dying of malaria. In pursuit of this goal, he undertook pharmacy studies in Mali and graduated with honors. Working as a young pharmacist, he was used to send a box full of antimalarial drugs including pills and injectables each year to his father who remained in the village with the rest of the family. In keeping with the African tradition of sharing the little one had, receiving these medications ensured prompt treatment of malaria cases within Djimdé’s family, extended family and friends, and the neighborhood. He quickly realized that, if his malaria actions were to reach beyond his community back home, he needed to do more. So, he volunteered his time at the Malaria Research and Training Centre at the National School of Medicine and Pharmacy in Bamako and later enrolled as a PhD student in microbiology and immunology at the University of Maryland, Baltimore.
The main highlights of Dr. Djimdé’s 30-year career are as follows.
1. Developing a molecular marker of chloroquine resistance
Chloroquine was a very effective treatment for malaria, and was also both safe and inexpensive, so it was used as an anti-malaria drug in areas across the world for many years. However, in the second half of the 1950s, Plasmodium falciparum, which gives rise to the worst, fatal symptoms among the malaria-causing protozoans that infect humans, gained resistance to chloroquine. The Pfcrt gene that causes chloroquine resistance in Plasmodium falciparum was later identified, but because strains cultivated 3 in labs were used for this research, it was not known whether Pfcrt was actually the causative gene of chloroquine resistance on the ground in areas with malaria epidemics in Mali. Together with his collaborators, Dr. Djimdé is the first to show that Pfcrt is the gene responsible for chloroquine resistance, even in endemic sites and designed a reliable molecular marker for chloroquine resistance in the field. His assay system was adopted first in sub-Saharan Africa, and later around the world. Under his leadership, the research team used that molecular marker to prove that chloroquine resistance was widespread in Mali, which led to a change in the first-choice treatment for malaria in the country.
2. Clinical development of antimalarial drugs
When Plasmodium falciparum, which had become resistant to chloroquine, was reported around the world, it became necessary to clinically introduce new, more effective antimalarial drugs. Dr. Djimdé and his fellow researchers carried out Phase II to IV clinical trials of artemisinin-based combination therapies (ACT) and verified their safety and effectiveness in sub-Saharan Africa. Artesunate-pyronaridine (PyramaxR), one of these ACT, had been registered as a malaria treatment drug 10 years earlier in Europe, but due to concerns about its safety its use was limited to one treatment per patient. However, in sub-Saharan Africa, children were infected with malaria multiple times each year. Effectiveness could not be expected with this administration of PyramaxR. Dr. Djimdé and his team carried out careful long-term cross-cutting research on a large scale, gathering 13,350 cases of malaria and treating them with one of four ACT, including PyramaxR, then following each case over two years. The outcomes showed that artesunate-pyronaridine was effective even when repeatedly administered to patients with consecutive episodes of malaria, and that there were no safety issues with multiple administration. This discovery led the WHO to approve multiple uses of PyramaxR. After this, PyramaxR came to be used in 27 countries, including 22 in sub-Saharan Africa, and has saved the lives of many African children.
3. Genetic diversity of African Plasmodia
Dr. Djimdé convinced his fellow researchers in 12 African countries to establish the Plasmodium Diversity Network Africa (now the Pathogens genomic Diversity Network Africa (PDNA) among 16 countries), and designed a system to easily share experimental protocols, samples, genetic data, and more. Joint research carried out through this network led to the first genetic research into malaria-causing protozoans across Africa, and Dr. Djimdé and his colleagues discovered the existence of major subpopulations of P.falciparum in sub-Saharan Africa. This research contributed to the WHO’s decision to 4 update its policy on malaria, which was previously not-country-specific, but rather handled in the same way in sub-Saharan Africa by taking a method suited to that country based on each country’s local data. Dr. Djimdé and his PDNA colleagues are continuing to work together to assess the potential impact of Plasmodium genetic diversity in response to malaria interventions, antimalarial drug resistance, vaccine effectiveness, and control of vector organisms.
4. Training young researchers through research
Dr. Djimdé is focused on creating a variety of programs to build research capacity in Africa and has spearheaded the formation of global strategic partnerships investigating malaria and drug resistance in the African region. Notably, as the founding director of Developing Excellence in Leadership and Genomics Training for Malaria Elimination (DELGEME) a training program he runs with his PDNA colleagues, he is committed to training excellent young researchers – for example, he has developed a wide-ranging training program on genetic and bioinformatics, including those of malaria-causing protozoans and human hosts, for young scientists from 17 sub-Saharan African countries. The young researchers who studied in DELGEME have produced numerous excellent research outcomes in the fields of genomics and bioinformatics. Recently, the program has been expanded into DELGEME Plus and is also stressing research into anti-microbial drug resistance under Dr. Djimdé ’s leadership.

Medical Services Category
Drugs for Neglected Diseases initiative (DNDi)
The Drugs for Neglected Diseases initiative (DNDi) was established in 2003 as a not-for-profit organization which develops safe, effective and affordable drugs and treatments for people afflicted by neglected diseases. (Photo credit: Brent Stirton Getty Images for DNDi)
Reasons for Award
There are so called twenty-one “neglected tropical diseases” that infect and afflict more than one billion people worldwide, but medicines that can treat them safely, effectively, and affordably have not been developed and manufactured due to market failures. To address this critical challenge with humanity and bravery, DNDi was founded in 2003 with the contribution of a portion of the Nobel Peace Prize awarded to the Médecins Sans Frontières (MSF). Since its inception, DNDi, along with its international partners, has developed and delivered 13 affordable new treatments for six deadly diseases, including African sleeping sickness, visceral leishmaniasis, pediatric HIV, and malaria, with broad impact in improving global health, particularly in lowand middle-income countries. Among these, fexinidazole, the first oral treatment developed by DNDi with its partners for the treatment of Gambian-type human African trypanosomiasis (gHAT, a form of African sleeping sickness), which is severely devastating in sub-Saharan Africa, has brought about a breakthrough effect in the endemic countries. In addition, through the HAT Platform, a network of research institutions and experts mainly from endemic countries in Africa, DNDi has helped overcome significant challenges such as conducting clinical studies in remote areas in accordance with international scientific quality standards. Based on these achievements, DNDi and its partners are working continuously toward the final target of the elimination of sleeping sickness.
Summary of Achievements
The Drugs for Neglected Diseases initiative (DNDi) was created in response to the frustration of clinicians and the desperation of patients faced with medicines that were ineffective, unsafe, unavailable, unaffordable, or that had never been developed at all. The Kenyan Medical Research Institute (KEMRI), the Indian Council of Medical Research (ICMR), the Oswaldo Cruz Foundation in Brazil, the Malaysian Ministry of 7 Health, and the Institut Pasteur of France, with the participation of World Health Organization Special Programme on Research and Training in Tropical Diseases (WHO/TDR), teamed up with MSF to found this organization.
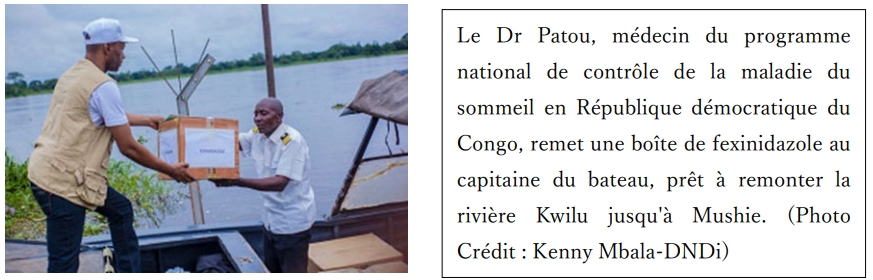
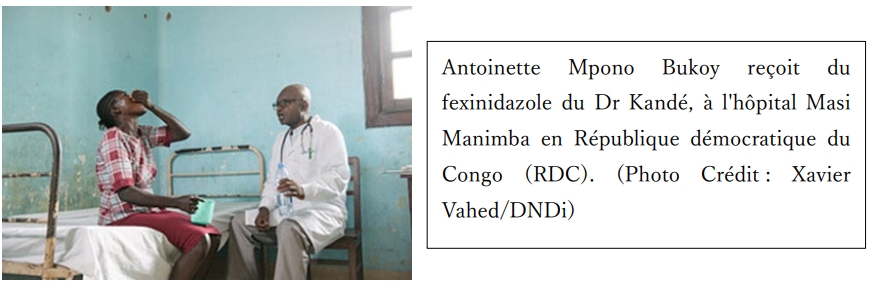
One remarkable example of DNDi’s achievement is the development and delivery of fexinidazole-the game-changing drug for T.b.gambiense sleeping sickness (gHAT) that killed hundreds of thousands of African people in the past century. People affected by this disease are some of the most vulnerable and live in some of the most remote and conflictaffected areas. For decades, its treatment was complex, difficult to administer, and even toxic. DNDi and its partners made continuous efforts, and developed and delivered fexinidazole, the first all-oral treatment for gHAT. It is an oral pill taken for 10 days, offering practical advantages over the previous standard of care, because it removes the need for systematic hospitalization and eases the burden on health systems, and leads to a reduction in the number of painful lumbar punctures for staging.
Fexinidazole was registered in the Democratic Republic of Congo in December 2018, where over 60% of sleeping sickness cases have been reported, and in Uganda in October 2021. In June 2019, fexinidazole was added to the World Health Organization (WHO) Essential Medicines Lists for children and adults. In August 2019, WHO published new sleeping sickness treatments guidelines to include fexinidazole as the first-line treatment for gHAT patients. All gHAT endemic countries are now utilizing fexinidazole as a firstline treatment.
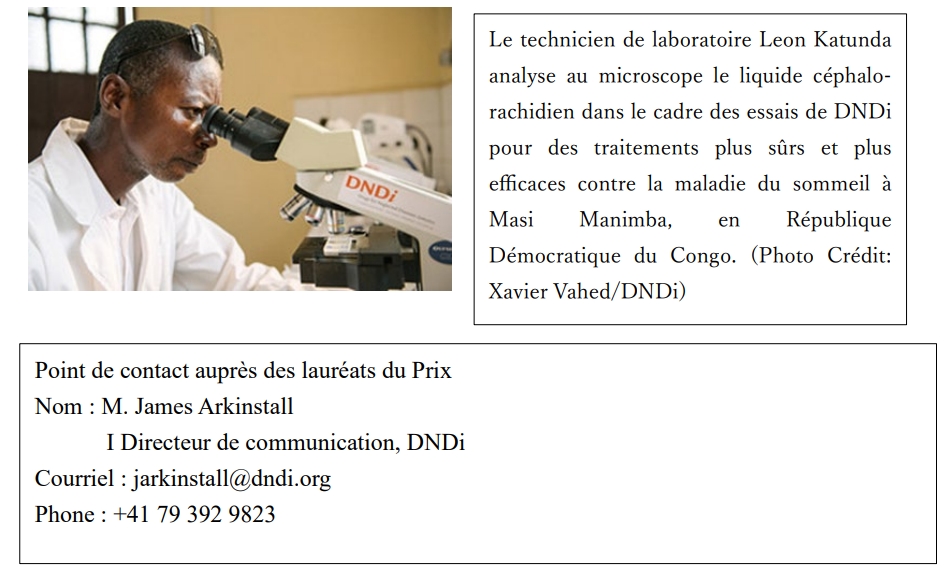
DNDi has been instrumental in making fexinidazole available to gHAT patients, partnering with Sanofi, WHO, the HAT Platform and national control programs in 8 endemic countries. Since 2005, DNDi has been supporting the creation and interactions of the HAT Platform, a network of 120 experts from more than 20 research institutions in endemic countries. DNDi’s close collaboration with national sleeping sickness control programs and the HAT Platform helped overcome the significant challenges to conducting clinical research in very remote settings in accordance with international ethical and scientific quality standards, facilitate access to and uptake of new treatments and advocate for an enabling policy and regulatory environment to meet the needs of the most neglected in endemic countries.
Bref dossier personnel de Dr. Abdoulaye Djimdé
[Date de naissance] le 6 Janvier, 1964 (en République du Mali)
Carrière d'éducation et de recherche
| Année | Description |
|---|---|
| 1982 | Baccalaureate, Lycée Publique, Sevare, Mopti |
| 1989–1993 | Pharmacist, Pharmacie Amani, B.P :9031 Bamako |
| 1993–1996 | Research Associate, Malaria Research and Training Center, Department of Epidemiology of Parasitic Diseases, National School of Medicine and Pharmacy, Bamako, Mali |
| 1996–2001 | Visiting Fellow, Laboratory of Parasitic Diseases, National Institute of Allergy and Infectious Diseases, National Institute of Health, Bethesda, Maryland, USA |
| 1988 | Pharmacy Doctorate, National School of Medicine and Pharmacy Bamako, Mali |
| 2000 | Master’s of Science, University of Maryland, Baltimore, USA |
| 2001 | Philosophy Doctorate, University of Maryland, Baltimore, USA |
| 2012 | Associate Professor, Parasitology and Mycology, CAMES |
| 2019 | Full Professor, Parasitology and Mycology, CAMES |
| 2001–présent | Head, Molecular Epidemiology and Drug Resistance Unit, Malaria Research and Training Center, Department of Epidemiology of Parasitic Diseases, Faculty of Pharmacy and Faculty of Medicine and Odonto-Stomatology, University of Science, Techniques and Technologies of Bamako, Mali |
| 2018–présent | Director, Malaria Research and Training Center, Department of Epidemiology of Parasitic Diseases, Faculty of Pharmacy and Faculty of Medicine and Odonto-Stomatology, University of Science, Techniques and Technologies of Bamako, Mali |
Honors and Awards
| Année | Récompense |
|---|---|
| 1996 | Doctoral Training Grant: Special Program for Research and Training in Tropical Diseases/UNDP/World Bank/WHO |
| 1996 | Visiting Fellowship: Laboratory of Parasitic Diseases/NIAID/NIH |
| 2001 | “Chevalier de L’Ordre National“, Republic of Mali |
| 2002 | Prize Fighting Malaria a Federation of the European Societies for Tropical Medicine and International Health and Sanofi-Synthelabo Award |
| 2004 | Senior Fellowship, European and Developing Countries Clinical Trials Partnership |
| 2005 | International Scholarship, Howard Hughes Medical Institution, Chevy Chase, Maryland, USA |
| 2007 | Caducee de la Recherche, Syndicat National des Pharmaciens d’Officine, Bamako, Mali |
| 2008 | « Prix de la Pharmacie francophone », National Academy of Pharmacy of France |
| 2012 | Wellcome Trust Sanger Institute, International Fellowship |
| 2012 | Professeur Agrégé, Parasitology and Mycology, XVIe Concours CAMES, Libreville, Gabon |
| 2015 | Co-Chair, Malaria Consultative Group on Drugs and Insecticides Resistance |
| 2015 | Commemorative Fund Lecturer, ASTMH 2015 |
| 2016 | Member, Board of Directors, American Society of Tropical Medicine and Hygiene |
| 2016 | Fellow, African Academy of Science |
| 2017 | Member, World Health Organization Malaria Policy Advisory Committee |
| 2018 | Fellow, Malian Academy of Science |
| 2020 | Honorary Faculty Wellcome Sanger Institute |
| 2021 | Fellow, The World Academy of Sciences |
| 2021 | Member, PLoS Scientific Advisory Committee |
| 2021 | Calestous Juma Research Leadership Fellow, Bill and Mellinda Gates Foundation |
| 2021 | Distinguished International Fellow, American Society of Tropical Medicine and Hygiene |
| 2021 | The Joseph Augustion LePrince Medal, for outstanding work in the field of malariology, America Society of Tropical Medicine and Hygiene |
| 2023 | Lauréat Prix Chrisophe Merieux, Institut de France |
Academic/ Professional Memberships and Other Professional Activities
| Année(s) | Organisation / Rôle |
|---|---|
| 1994 | Member, African Society of Parasitology |
| 1994 | Member, Medical Society of Mali |
| 1996 | Member, American Society of Tropical Medicine and Hygiene |
| 2005–2014 | Member, Scientific Advisory Board, WWARN |
| 2007 | Founding Coordinator, West African Network for Clinical Trials of Anti-Malarial Drugs, WANECAM |
| 2011 | Member French Society of Parasitology |
| 2014 | Member, WHO Expert review group on molecular marker of artemisinin resistance k13 |
| 2015 | Founding Director, Developing Excellence in Leadership and Genomics Training for Malaria Elimination in Sub-Saharan Africa (DGLGEME) |
| 2016-2024 | Member, WHO Malaria Policy Advisory Group (MPAG) |
| 2017 | Founding President, African Association for Research and Control of AntiMicrobial Resistance (AAAMR) |
| 2020 | Founding President, Pathogens genomic Diversity Network Africa (PDNA) |
The Major Publications of Dr. Abdoulaye Djimdé
1. Djimdé A et al., A molecular marker for chloroquine-resistant falciparum malaria.
New England Journal of Medicine 344:257-63 (2001)
2. West African Network for Clinical Trials of Antimalarial Drugs (WANECAM).
Pyronaridine-artesunate or dihydroartemisinin-piperaquine versus current first-line therapies for repeated treatment of uncomplicated malaria: a randomized, multicenter, open label, longitudinal, controlled, phase 3b/4 trial. Lancet 391:1378-1390 (2018).
3. K13-propeller polymorphism in Plasmodium falciparum parasites in sub-Saharan Africa. E.Kamau et al. (16 authors) Djimdé A. J Infect Dis. 243:1352-1355 (2015)
4. Ghansah A, (17 co-authors), Kwiatkowski DP, Djimdé AA. Monitoring parasite diversity for malaria elimination in sub-Saharan Africa. Science. 345:1297-8 (2014)
5. Amambua-Ngwa A, (19 co-authors), Djimdé AA. Major subpopulations of Plasmodium falciparum in sub-Saharan Africa. Science 365:813-816 (2019)
Brief Organizational Record of Drugs for Neglected Diseases initiative (DNDi)
Essentials of the Organization
Established in 2003 in Geneva. DNDi develops and delivers drugs and treatments for neglected disease in collaboration with 8 regional offices worldwide and over 200 industrial, governmental and academic partners.
Honors and Awards
| 2008 | Goodwin Award |
| 2008 | Société de Pathologie Exotique Golden Medal |
| 2012 | BBVA Foundation |
| 2013 | The Rockefeller Foundation |
| 2013 | Carlos Slim Foundation |
| 2014 | FINEP Award for Innovation |
| 2014 | Corporate Social Responsibility Alliance Excellence Award |
| 2017 | Prix 2017 de l’Innovation |
| 2018 | Anne Maurer-Cecchini Award |
| 2020 | Else Kroner Fresenius Award for Development Cooperation in Medicine |
| 2020 | Grand Prix, WHO Health for All Film Festival |
| 2020 | Golan Christie Taglia Patient Impact Philanthropy Award |
| 2021 | French National Order of Merit |
| 2020-2021 | Prince Mahidol Award |
| 2021 | Prix Galien Africa |
| 2023 | Princess of Asturias Award for International Cooperation |
Major Publications
The publications listed below represent a selection of DNDi’s extensive research on sleeping sickness, with a focus on Access/Implementation.
(Articles)
1. Development and introduction of fexinidazole into the Global Human African Trypanosomiasis Program. Valverde Mordt O, Tarral A, Strub-Wourgaft N. The American Journal of Tropical Medicine and Hygiene 2022; tpmd211176.
2. Latest advances in control of sleeping sickness: Towards elimination. Valverde Mordt 14 O. Bulletin of the Netherlands Society for Tropical Medicine and International Health 2020:6-8
3. How clinical research can contribute to strengthening health systems in low resource countries. Mbo F, Mutombo W, Ngolo D, Kabangu P, Valverde Mordt O, StrubWourgaft N, Mwamba E. Tropical Medicine and Infectious Diseases 2020, 5(48)
4. Registering new drugs for low-income countries: The African challenge. Moran M, Strub-Wourgaft N, Guzman J, Boulet P, Wu L, Pecoul B. PLos Medicine 2011, 8(2). E1000411
5. NECT is next: Implementing the new drug combination therapy for Trapanosoma brucei gambiense sleeping sickness. Yun O, Priotto G, Tong J, Flevaud L, Chappuis F. PLoS Negl Trop Dis, 2010, 4(5) :e720
(Conference Presentation)
1. ISNTD d3 (June 29, 2022) Disease focus: sleeping sickness, de-risking discovery through partnerships and driving sustainability through access. Webinar including Florent Mbo and François Bompart.
2. EDCTP Forum (November 7, 2023) Poster number 580 on Capacity development to facilitate the delivery and uptake of a new medical intervention: fexinidazole oral treatment for the elimination of human African trypanosomiasis with DNDi authors Florent Mbo, Olaf Valverde Mordt, Digas Ngolo, Albert Nyembo, Alphonsine Bilonda.
(Textbooks/Miscellaneous)
1. Human African trypanosomiasis (sleeping sickness): The road to elimination revisitedachievements and remaining challenges
(END)
- Log in to post comments